Bringing full insurance and billing services to behavioral health facilities.
Our team comes from various backgrounds in the inpatient addiction and mental health industry. We know well the urgency that governs all parts of the process—for treatment centers, insurance providers, and concerned families alike.
This urgency demands a comprehensive, collaborative, compliant approach. We handle the entire approach and work with your clinical team only when needed so you can focus on providing quality treatment for your patients.
We are committed to a simple philosophy: a comprehensive, collaborative, compliant approach to insurance billing.
We are committed to a simple philosophy: a comprehensive, collaborative, compliant approach to insurance billing.
Our Services Include:
For Treatment Programs
Bringing full insurance and billing services to behavioral health facilities.
Our team comes from various backgrounds in the inpatient addiction and mental health industry. We know well the urgency that governs all parts of the process—for treatment centers, insurance providers, and concerned families alike.
This urgency demands a comprehensive, collaborative, compliant approach. We handle the entire approach and work with your clinical team only when needed so you can focus on providing quality treatment for your patients.
We are licensed insurance professionals governed by a strong code of ethics. We have a genuine interest in cultivating long-term, productive relationships with all those involved in the industry.
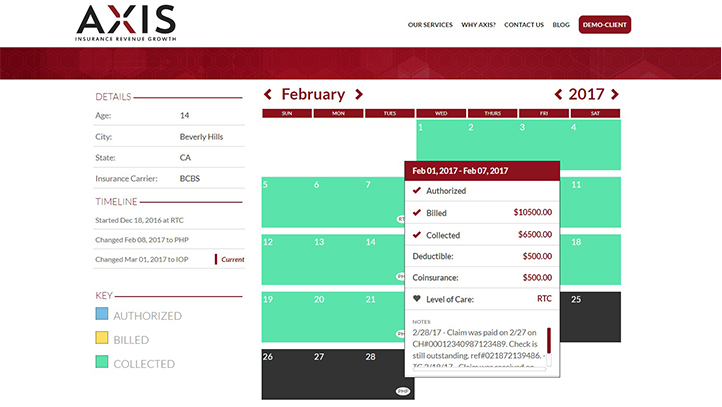
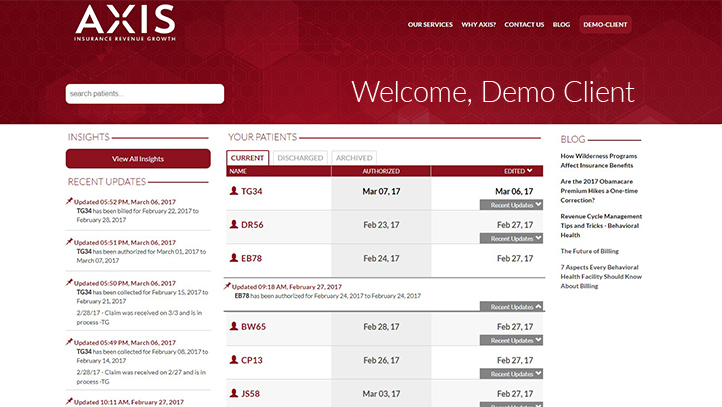
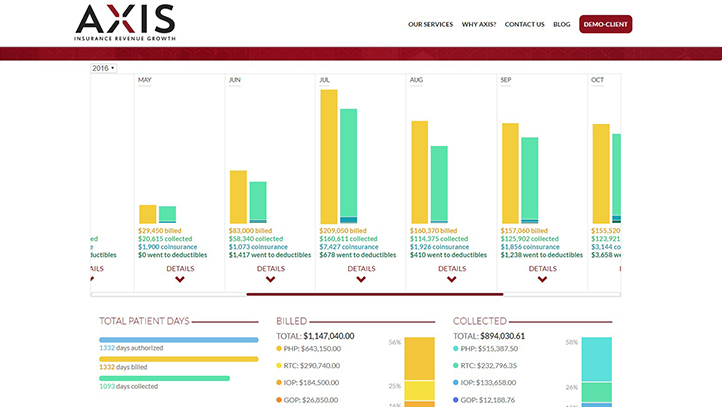
We communicate with, assist and support families during the appeals process, based on their specific needs. Through our web portal, we ensure transparency for patients and facilities, ensuring that both know exactly what is being done.
We don’t get paid unless you do. Our unique partnering system ensures that all involved parties work together to achieve a result that meets everyone’s needs.
For Ed Consultants and Referring Professionals
What is your reimbursement strategy?
We engage your insurance benefits to maximize potential reimbursement for the policy you pay for on a monthly basis.
What are the pros and cons of your reimbursement strategy?
The pros for using Axis are that we do not have an up front fee and only get paid when you do. Also we have been in the insurance industry for the past 20 years and are aligned to maximize potential reimbursement. Axis strategy is in lock step with your insurance rules and regulations for reimbursement to the point where there are no cons when choosing Axis.
How much reimbursement might I anticipate?
Depending on your particular insurance & medical necessity Axis has seen 30%-40% of your out of pocket expense reimbursed.
What is your process for working with families and their residential / wilderness therapy claims?
Axis best approach with families is to be engaged prior to any admission of a facility or wilderness program. The first step is to verify your benefits to see if there is any potential reimbursement. Second is to coordinate with the program the admission date to get all necessary clinical information to engage your insurance. Third is to get authorization for coverage and send claims to your insurance as each authorization is obtained. The last step in the process is finalizing claims either through the family or the facility for accounting and then finally reimbursement for invoicing.
How do you approach and support preauthorization?
Axis approaches pre authorization the best at the time of admission. This is very key when engaging insurance carriers. It is very difficult to obtain days or months after admission. In supporting pre authorization Axis will do weekly update calls with case managers to maintain ongoing coverage until medical necessity has been exhausted.
How do you define success? What is your success rate?
Axis defines success in two ways, one is giving clear information on how your insurance works and if there is potential for reimbursement. Second is when there is reimbursement to help offset the costs of treatment. Dependent on your insurance out of network benefits is the driver for success rate. As long as you have out of network benefits Axis will be able to get reimbursement that your policy allows.
What is your fee structure and when am I billed?
Axis fee structure is 10% of any reimbursement accrued to your insurance. Axis sends out invoices once proof of payment has been allotted to families or facilities.
How are you different than other insurance advocates?
Axis is to date the only insurance advocate firm that has licensed insurance professionals on staff.
How long does the insurance reimbursement process take?
On average it takes 45-60 days for claims to be processed by the major insurance carriers.
Do you process claims using my disability insurance?
No, disability insurance does not cover any residential or wilderness admissions.
For Families / Members
Below is general information about Insurance Advocates for residential programs including therapeutic boarding schools, residential treatment centers, and wilderness therapy programs. It is worthwhile to have a professional review your policy to understand what reimbursement you may anticipate. Contact information for three Insurance Advocates is included below.
As a general rule, wilderness therapy is excluded in most policies. This does not mean that you are not potentially eligible for some degree of reimbursement. While not a guarantee, families are increasingly being reimbursed a percentage of program costs, though 100% is extremely rare.
The nuances of the insurance industry are vast. Portions of TBS/RTC treatment can be billed directly or reimbursed. Many programs require private pay options up front with support of Super Bill for reimbursement afterwards. Most TBS/RTC’s are not in-network. Please be sure to understand how each program works with insurance and Insurance Advocates.
Families that attempt to process claims on their own for wilderness are denied coverage over 90% of the time. TBS/RTC’s have a wide range of insurance participation. I strongly recommend families work with an Insurance Advocate that offers experienced professionals and services to navigate the nuances of your specific insurance plan and the claims process.
Insurance Advocates manage health insurance claims to help you develop and implement a strategy to achieve maximum coverage. They will provide a free initial consultation, perform a verification of benefits, support any preauthorization requirements, and address all correspondence with your insurance company including coding, claim creation, electronic claim submission, corrections, appeals and denials.
We recommend contacting an Insurance Advocate prior to enrollment. This ensures that your policy will be professionally reviewed with a verification of benefits completed so can know what to expect from your insurance plan and understand your reimbursement strategy. If you are unable to contact an Insurance Advocate before enrollment, we advise you contact one as soon as possible.
No, each Insurance Advocate offers differing strategies, services, and fee structures. Fee structures include hourly, flat fees, and percentage of reimbursement. It is up to the family to determine which Insurance Advocate best aligns with your goals.