The reality
It’s a typical Friday morning, birds chirping, blue skies and sun is shining. The only thing on my mind was if I was going to work at home or to set up shop on the beach because I could already feel the heat coming in from my open window. As I do my morning ritual, which is to check all my social media platforms, (hopefully I’m not the only one who does this), the first thing I see is a post saying, “Anthony Bourdain, world-traveling chef, and TV star, dies at 61 in an apparent suicide.”
Immediately all I could think of was how influential he was to me in particular. I’m an aspiring chef, and of course, I enjoy writing and love seeing the world through the eyes of those who are not like me. Anthony Bourdain embodied all of these qualities and more, and then shared them with the whole world so they could see, feel, taste and touch different cultures in ways we never thought were possible.
I believe he did this because he was a true humanitarian. He was unbelievably intelligent with his articulation and pulling in your attention, also one of the most real and raw speaking public figures I’ve ever seen on television. Please don’t get me wrong, I’m not comparing it to those reality shows that have no substance or positive influence, you know what I’m talking about..take your pick.
I say all of this to point out, that we as “humanity”, lost a very significant influential character that strived to make our world a better place to live, make us feel more alike than different, and showed us it’s ok to know the unknown. No pun intended.
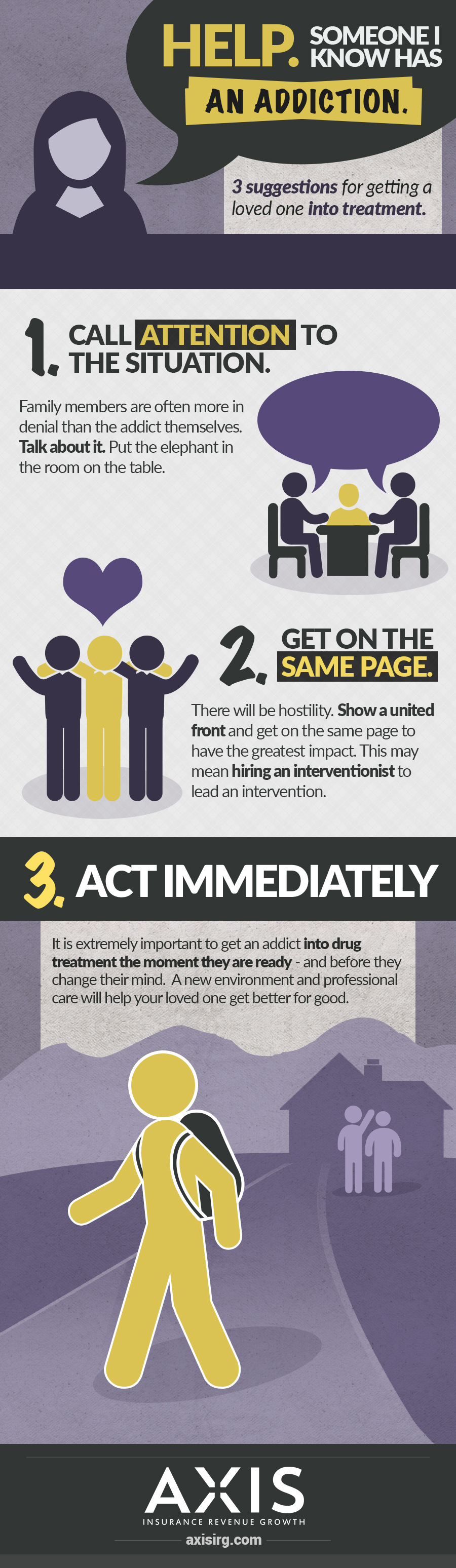
So now let’s talk about the real problem at hand. The elephant in the room that everyone knows is there and continues to grow bigger and bigger as we speak. Suicide! Just days before Anthony Bourdain’s death, successful and well-known American fashion designer, Kate Spade, took her life also. It’s a reality that has become a loud cry for help.
We can’t forget that not all suicides get the publicity like celebrities’ get. Normal families across the nation are losing loved ones because of this very serious problem. Rather it is due to substance abuse, mental health, or whatever…there is no explanation good enough that could justify taking your own life.
We sometimes think that we have to emulate and try and live this, “perfect life”, and are ashamed or scared to talk about our problems with someone. Just like anything that you plant, that bad seed is going to continue to grow and start to invade every aspect of your life if you realize it or not. That’s one reason why it’s so important to discuss your problems with an outside perspective. A lot of the times we lose sight or get so submerged in the maze, we need that light at the end of the tunnel so we know what direction to head.
The numbers
The CDC (Centers for Disease Control and Prevention), analyzed the increase of suicides in the United States, using data from the National Vital Statistics System research from 1999 to 2016, and shows that suicide has increased 25%. This includes twenty-five states experiencing a 30% rise in suicides across the nation.
Dr. Anne Schuchat, principal deputy director of the CDC, states that more than half of those who died from suicide were not even medically diagnosed with a mental health condition.
Her statement is a rude awakening and hits close to home for all of us. If we don’t intervene, these numbers will, unfortunately, reach catastrophic numbers.
Just in 2016 alone, 45,000 deaths were lost to suicide. Taking a look at individual states Delaware ranging from a 6% increase and nearly a 58% increase in North Dakota, researchers say.
Data collected from the National Violent Death Reporting System shows that 54% of individuals who committed suicide in 2015 did not even have a mental health condition. What’s more alarming is, researchers found that different circumstances such as relationship problems or loss of someone triggered more suicides than those who were medically diagnosed with a mental health condition.
Get help
We are all vulnerable to this reality, and we need to be there for those who need it and when they need it. If you notice someone may be dealing with this problem, speak up and talk about it. There are professional, confidential and friendly organizations that can help. Places like the National Suicide Prevention Line, are here to help those who need it. You can also call 1-800-273-8255, and they are available 24/7 every day.
If you want to reach out to a Mental Health facility, do your research to see which one will be the best fit for yourself or whoever is seeking help. Hundreds of treatment centers across the United States, for you to choose from, and they all have well-qualified therapists and doctors that are trained to get your life back.
Awareness of this topic can never go unknown, and you can help by re-posting, commenting, by just starting a dialogue on your social media platforms may just save someone’s life.


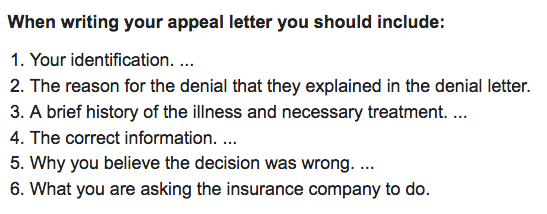 A common occurrence with insurance claims is that they are either fluctuating and underpaying or not paying at all. If someone is not
A common occurrence with insurance claims is that they are either fluctuating and underpaying or not paying at all. If someone is not